Sacroiliac Joint Pain: Comparing Intra-Articular Steroid Injections and NSAIDs
In patients without sacroiliitis, without a history of lumbar surgery, and with less than 30 days of pain oral NSAIDS are advantageous.
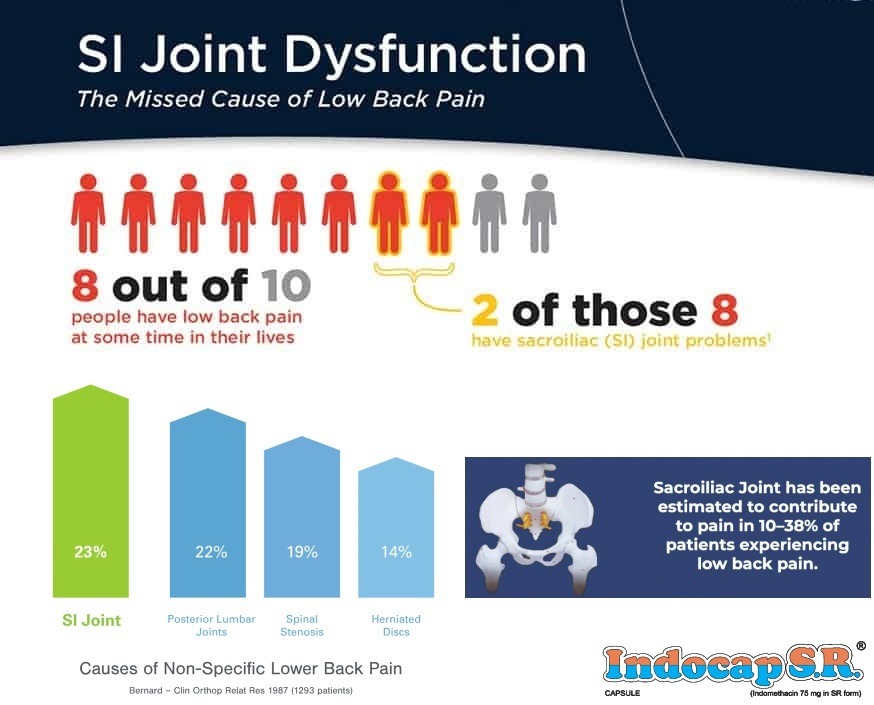
The sacroiliac joint, one of the most significant contributors to axial low back pain, supports the entire spinal load. The incidence of pain localized to the sacroiliac joint rises with age with tenderness in the sacroiliac joint documented in 15-30% of outpatient cases of low back pain.
A recent prospective study of 60 outpatients receiving NSAIDS (including 25mg indomethacin OD) or sacroiliac injection revealed similar reduction in VAS scores at the end of the first month in group on NSAIDs in patients without sacroiliitis, without a history of lumbar surgery, and with less than 30 days of pain.
In patients with sacroiliac joint pain, sacroiliac joint injection was superior to NSAIDs for pain relief in those with pain for more than 30 days, those with MRI-diagnosed sacroiliitis, and those who had undergone lumbar surgery.
One significant factor in pain of the sacroiliac joint is elevated levels of cytokines that result from an inflammatory reaction. The main goal is to decrease inflammation and prevent the production of cytokines. To achieve this, NSAIDs with strong anti-inflammatory properties can be used orally. Corticosteroids, on the other hand, work by antagonizing the immune response. However, the effects in the short term are limited to its anti-inflammatory activity. Over an extended period, these facilitate the upregulation of anti-inflammatory genes while downregulating pro-inflammatory genes, such as cytokines.